About
Population Health Management is a discipline within health care that studies and delivers care across a specific group of people. It aims to improve the health and quality of life for a targeted group of patients. This is done through comprehensive care coordination, data analytics, risk stratification (high risk, low risk, rising risk), and interventions targeted at the individual, group, and community levels. Please contact
phm@ahca.org with questions and inquiries.
PHM models vary based on the degree of risk, degree to which payment is tied to quality, reliance on data analytics, and level of care coordination.
Comparison of PHM models
| Low | Provider-Owned Networks
| These Integrated Care Networks are joint ventures of independent providers coming together to negotiate value-based reimbursement that focuses on efficiency and quality outcomes.
|
| Moderate | Bundled Payments or Episode of Care Models
| A single payment for all care and services provided for a specific patient performed by multiple providers for a single procedure or medical condition over a specified period of time. Focused on certain conditions, bundled payments tend to have a specialty/hospital-centered approach. |
| Moderate | Accountable Care Organizations (ACOs)
| Networks of physicians, hospitals, and other health care providers that voluntarily come together to coordinate care and manage the total costs of care of a population. ACOs share in the financial risks and rewards of performance against benchmarks and on patient outcomes. It includes all conditions and has a primary care-centered approach. There are different Medicare ACO models with varying degrees of risk and Medicaid ACOs. |
| High | Direct Contracting
| Broadens participation by allowing a varied group of participants, including health plans who form a Direct Contracting Entity (DCE), to contract with CMS under a capitated per beneficiary, per month payment for the cost of care for the beneficiary. Different from previous Center for Medicare and Medicaid Innovation models, participant providers (physicians) are paid by the DCE and not CMS, but providers still submit claims.
|
| High | Provider-Owned Special Needs Plans
| Special Needs Plans (SNPs) are Medicare Advantage plans (Part C) that limit enrollment to subgroups of Medicare beneficiaries with specific needs (i.e. institutionalized individuals, dual-eligible individuals, or individuals with certain chronic conditions as specified by CMS). SNPs offer services tailored to the specific population under a National Committee on Quality Assurance-approved model of care and must provide Medicare prescription drug benefits (Part D). Plans are sometimes referred to as “provider-led” or “provider-owned” SNPs.
|
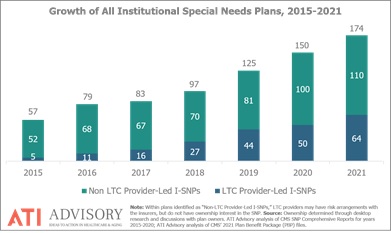
Provider-Led Special Needs Plans: One PHM Growing Solution
Special Needs Plans (SNPs) are Medicare Advantage plans focused on specific sub populations. There are three types of SNPs.
-
Institutional Special Needs Plans (I-SNPs)/Institutional Equivalent Special Needs Plans (IE-SNPs): I-SNP-eligible individuals are Medicare beneficiaries that reside or are expected to reside in a nursing facility (NF) for 90 days or more. IE-SNP-eligible individuals are Medicare beneficiaries that reside in their own homes that meet (and continue to meet) a NF level of care as determined by the state assessment.
-
Dual Eligible Special Needs Plans (D-SNPs): Eligible individuals must have Medicare and Medicaid.
Providers are now leading SNPs, particularly I-SNPs, which benefit their long term care (LTC) residents.
In 2019, AHCA/NCAL formed the Population Health Management Council to convene and support long LTC providers who are leading in PHM initiatives through advocacy, education, and quality improvement data. Along with AHCA/NCAL provider members, there are organizations whose sole or primary purpose is to partner with LTC providers to support LTC provider ownership interests in PHM models. AHCA/NCAL has four such Council Partners, and more information about each is available below.