Stronger Centers for Medicare and Medicaid Services Oversight of Medicare Advantage Plans is Needed as Enrollment Grows
More protections for Medicare beneficiaries are needed due to rapid growth in Medicare Advantage (MA) Plan enrollment. From 2021 – 2022, enrollment increased by double digits in 33 states. Congress, as well as a growing number of federal agencies and media outlets, also are highlighting challenges.
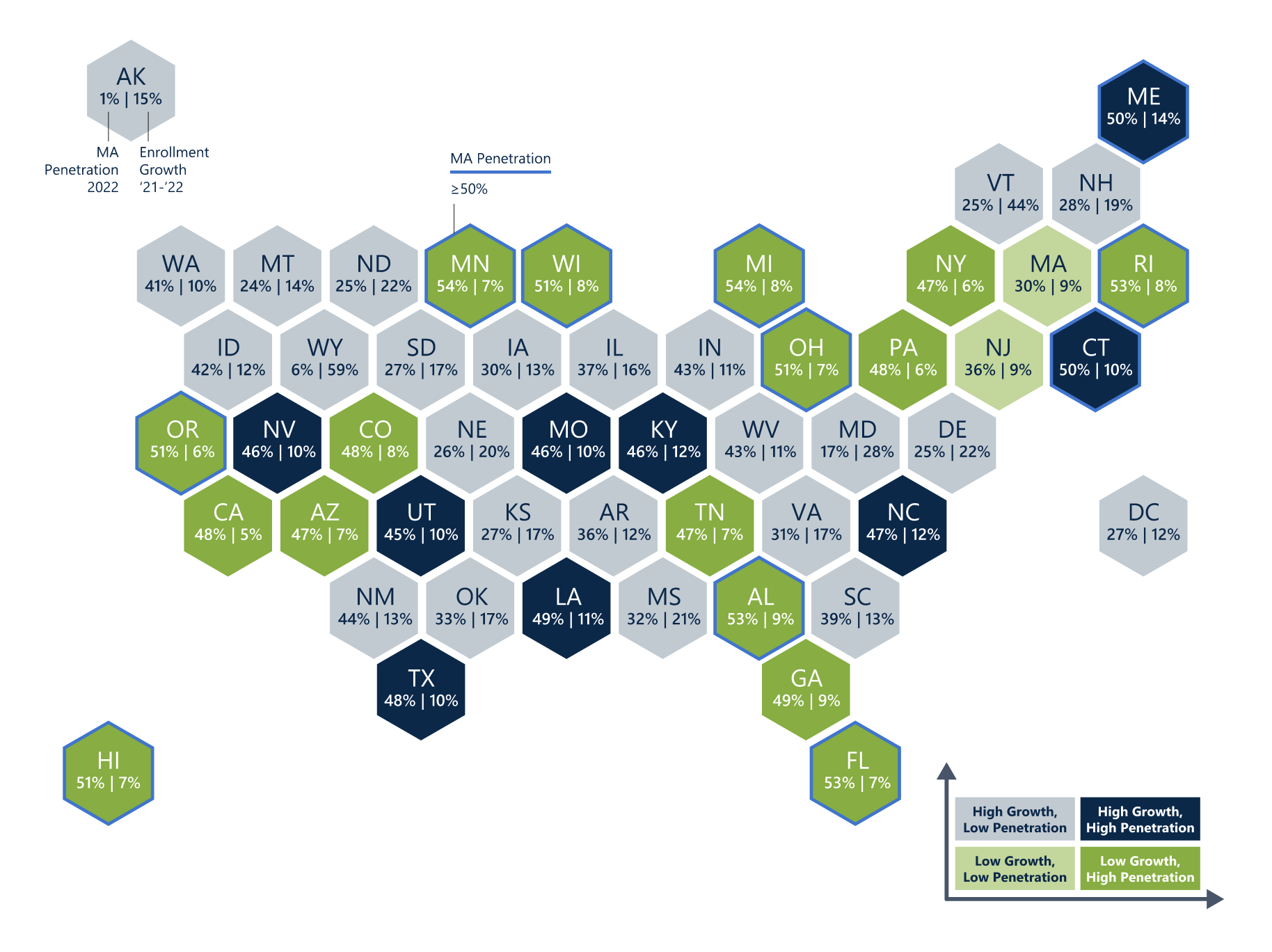
Source: The Chartis Group, Medicare Advantage Enrollment Continues to Surge in an Increasingly Complex and Competitive Landscape
Additionally, total MA Plan enrollment has grown at a pace more rapidly than projected by federal agencies with more beneficiaries enrolling in MA than in traditional Medicare. With more Medicare beneficiaries enrolling in MA than in the past, CMS should increase its oversight to ensure access to all needed services and care.
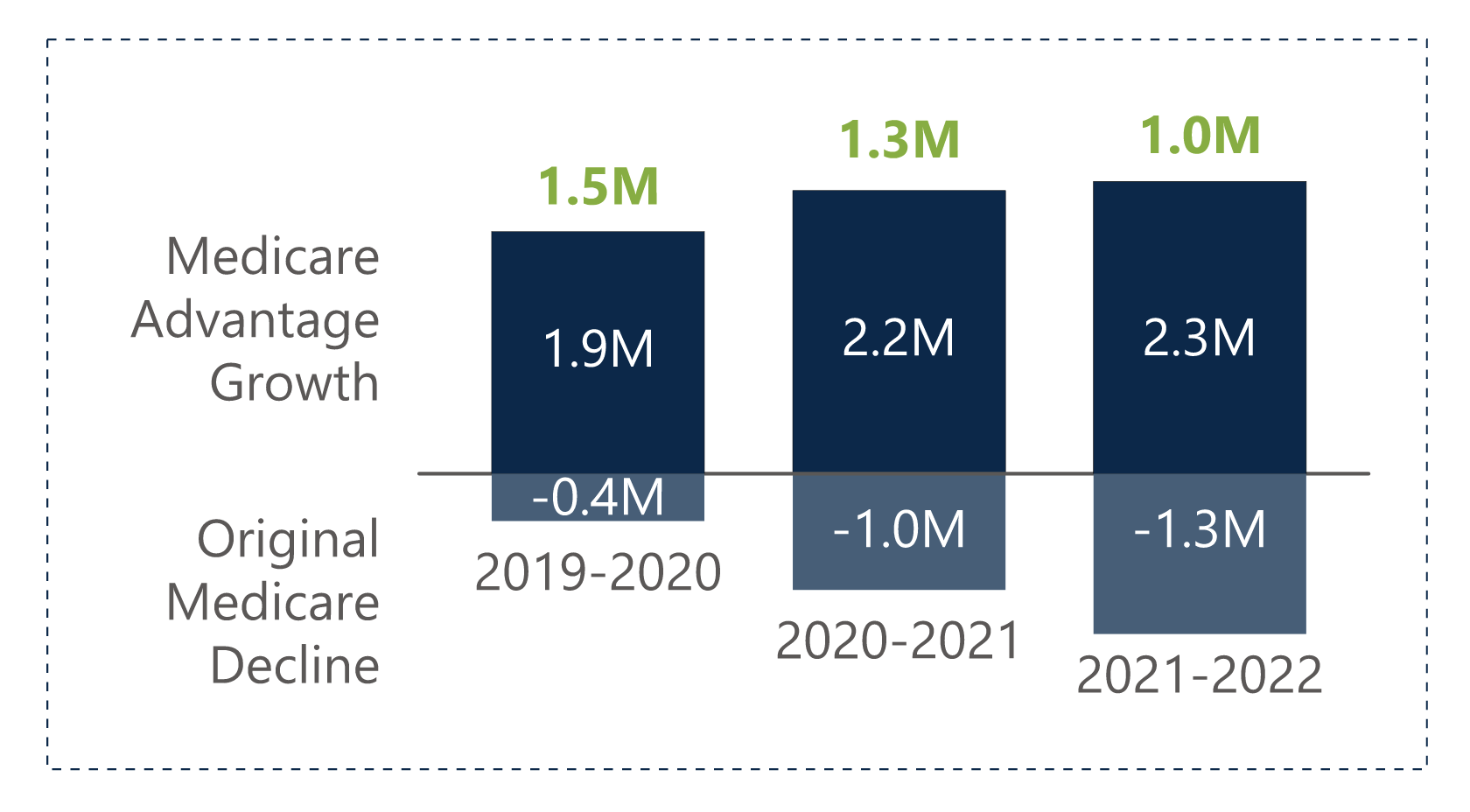
Source: The Chartis Group, Medicare Advantage Enrollment Continues to Surge in an Increasingly Complex and Competitive Landscape
Already struggling providers report notable challenges with MA Plans, which now cover far more SNF Medicare days while paying less for those days. Challenges include:
- MA Plans often pay outside of federally required timelines and create administrative complexities which jeopardize care.
- Research raises new questions about the cost effectiveness of Medicare Advantage.1
- Providers and beneficiaries have inadequate avenues and options for communicating with federal officials on challenges associated with MA plan coverage and operations.
- Stronger provisions are needed to ensure plans comply with federal requirements for important functions related to ensuring access to needed services (i.e., prior authorizations, timely processing of grievances and appeals). Legislation was recently introduced to address prior authorization challenges.
- Federal government rarely significantly engages in plan corrective action.
States and Congress have called on CMS to revisit MA plan
marketing guidelines, and CMS has released a
proposed rule placing new provider and beneficiary protections associated with prior authorizations and denials. But much more is needed.
As enrollment has grown, an array of media outlets have begun covering MA Plan challenges faced by beneficiaries and providers. AHCA/NCAL will be posting regular summaries of media coverage. For more information on MA Plans, contact Nisha Hammel or Martin Allen.
_______________________________________
1Duggan, M., et. al.
Who Benefits When the Government Pays More? Pass-Through in the Medicare Advantage Program. National Bureau of Economic Research. March 2014.